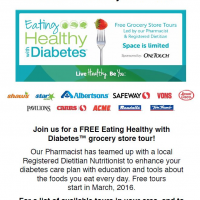
Navigating through a grocery store can be a challenge, especially if you are newly diagnosed with diabetes and/or are trying to start a new healthy eating plan. Understanding food labels, knowing what foods to purchase, and how to plan healthy meals may feel like road blocks on your path to the grocery store checkout counter without a solid […]